The UBC internal medicine program recognizes that developing ultrasound training has many benefits and aims to be a leader in this area.
- First, we recognize that training in bedside ultrasound can enhance the clinical examination and improve patient care.
- Second, ultrasound can serve as a powerful teaching tool and therefore, may serve to improve the delivery of non-ultrasound clinical skills.
- Third, medical schools are beginning to incorporate ultrasound into pre-clinical training and these future residents will be looking for post-graduate training that can accommodate their ultrasound learning needs.
- Last, the internal medicine program can seize the opportunity to contribute to research in the use of point of care ultrasound.
The UBC internal medicine program aims to create opportunities for development of ultrasound skills that will prepare the learner for clinical practice. Our goals are making instructors available so they can help learners grow their skills, providing access to ultrasound machines and learning resources that allow learners to practice, and developing evaluation materials in order to recognize those learners who have achieved a satisfactory level of competence. In addition, we aim to stay involved with national initiatives within the ultrasound community and contribute to incorporating ultrasound at the level of the Royal College.
Point of Care Ultrasound is an exciting addition to clinical medicine with incredible potential. We aim to harness the multitude of benefits and will deliberately and carefully work towards delivering those advantages to residents in internal medicine at UBC.
Point of Care Ultrasound (PoCUS) differs from traditional diagnostic ultrasound in many ways. It’s definition is still debated, but there are several key distinguishing characteristics:
- PoCUS is performed by the clinician at the point of care as part of the standard clinical assessment
- PoCUS is a limited, goal directed exam guided by a specific clinical question
- PoCUS exams may be single system or multi system involving more than one application
- PoCUS provides additional data points when there is diagnostic or therapeutic uncertainty after reviewing the available clinical information
- PoCUS can be used to follow a patient over time to monitor treatment interventions or changes in patient status
- PoCUS is NOT a stand alone investigation… the information obtained during a PoCUS exam must be interpreted as part of the clinical picture
- PoCUS is NOT a comprehensive diagnostic tool and does NOT replace a diagnostic ultrasound
The PoCUS literature has demonstrated that it has the potential to provide a wealth of information to the clinician at the 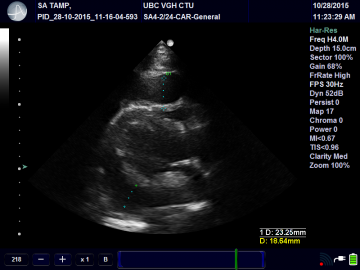 bedside.
bedside.
It has been shown to:
- improve the accuracy of bedside diagnosis
- alter therapeutic decision making
- improve the safety of bedside procedures: This technology has been embraced by multiple disciplines including Emergency Medicine, Critical Care and Anesthesia, to name a few. Research has revealed the feasibility of numerous applications for the bedside clinician and many of these are relevant to internal medicine. Although its role in basic bedside procedures has clearly been established in Internal Medicine, its use in daily clinical practice has not yet been universally accepted.
How is PoCUS used in internal medicine?
PoCUS is utilized in internal medicine both from a diagnostic and therapeutic standpoint. Diagnostically, PoCUS can be used to obtain additional information to help sort out challenging cases. The exam is often approached from the perspective of a problem of uncertain cause. Common clinical scenarios encountered in internal medicine for which PoCUS is often helpful are:
- Hypotension or shock NYD
- Dyspnea or hypoxia NYD
- Chest pain NYD
In the instance of new hypotension of unclear cause, a limited cardiac, IVC and DVT scan may be employed. A hyperdynamic heart with normal LV systolic function and a normal RV:LV ratio with an IVC collapsibility index of 80% and completely compressible Femoral and popliteal veins suggests a hypovolemic or distributive cause for the patient’s hypotension. Of course this would need to be carefully integrated into the rest of the clinical picture.
PoCUS also improves safety, success and operator confidence for many of the common bedside procedures in internal medicine. Ultrasound is used to mark sites for thoracentesis, paracentesis and even lumbar puncture when landmarks are difficult to palpate. Ultrasound can be used to allow for direct needle visualization in procedures such as CVC, peripheral and arterial line insertions as well as arthrocentesis.
PoCUS applications relevant to Internal medicine include:
Clinical applications to aid in diagnosis and guide management:
- Lung ultrasound
- Interstitial syndromes (eg. pulmonary edema)
- pleural effusions
- consolidation
- pneumothorax
- Cardiac ultrasound
- LV systolic function
- RV assessment
- pericardial effusions
- gross valve lesions
- Assessment of IVC and JVP
- DVT
- Ascites
- Splenomegaly
- Hydronephrosis
- Bladder distension
- Skin abscess
- Joint effusions
Procedural applications:
- Thoracentesis
- Paracentesis
- Central line insertion
- Peripheral line insertion
- Arterial line insertion
- Lumbar puncture
- Arthrocentesis
UBC Internal Medicine Point of Care Ultrasound (PoCUS) Training
| Year 1 |
I. Bootcamp
- Introduction to PoCUS Lecture
The focus of the initial lecture is to:
- introduce the resident to the scope of PoCUS in internal medicine
- introduce the resident to the PoCUS curriculum and learning resources at UBC
- provide a roadmap for learning PoCUS during residency
Hands on ultrasound workshop number 1
The aims of the first of three hands on workshops in the first year are:
- introduce the resident to basic knobology
- introduce the resident to strategies for image acquisition and optimization
- introduce the resident to using PoCUS to identify the height of the JVP
- introduce the resident to using PoCUS for procedural guidance
- identifying ascites and guidance for paracentesis
- identifying pleural effusions and guidance for thoracentesis
- identifying the IJ and guidance for CVC insertion
- needle visualization
II. Hands on ultrasound workshop number 2
The aims of the second of three hands on workshops in the first year are:
- introduce the resident to IVC scanning
- Introduce the resident to clinical integration of IVC
- introduce the resident to a systematic protocol for scanning the lungs
- introduce the resident to the 4 fundamental lung ultrasound findings
- A-lines as an indicator of a soft tissue air interface
- B-lines as an indicator of interstitial pathology
- pleural effusions
- soft tissue appearance of lung consolidation and atelectasis
- introduce the resident to clinical integration of lung scanning
III. Hands on ultrasound workshop number 3
The aims of the final hands on workshops in the first year are:
- introduce the resident to the 4 basic cardiac views
- introduce the resident to a systematic method of assessing each view
- introduce the resident to pitfalls associated with cardiac scanning
IV. Junior resident teaching on CTU
Junior teaching will occur on a weekly basis when the resident is on resident is on a CTU rotation. When a PoCUS literate faculty member is available we will aim to provide one PoCUS session. The aims of the Junior teaching session will be to find a patient with pathology and demonstrate how PoCUS findings can be implemented clinically.
V. On-line learning
The Internal Medicine Point of Care Ultrasound website on UBC ConnectThis website is meant to serve as the central repository for information and learning resources related to the internal medicine PoCUS curriculum. This website should be visited regularly to help guide ultrasound related activities and find learning resources such as podcasts.
Information on this website includes:
- schedule to help organize your ultrasound learning activities
- references for machine operation and image archiving
- targets for ultrasound images (suggested quotas)
- information about image content (minimum criteria)
- helpful podcasts
- examples of images
- interesting ultrasound cases
- important literature
VI. Image archiving and QA (under construction)
Our goal is to establish a central repository for images obtained by residents that can be reviewed by expert faculty. This will provide the opportunity for quality assurance as well as feedback on-line. I am aiming to have this available in the 2019/20 academic year.
| Year 2 and 3 |
I. Hands on ultrasound workshop number 4 (Under construction)
The aims of the first hands on workshops in the second year are:
- review principles of lung scanning
- introduce more advanced lung interpretation including pleural line abnormalities and complex pleural effusions
- review 4 basic cardiac views
- introduce cardiac ultrasound assessment for LV systolic function and pericardial effusions
II. Hands on ultrasound workshop number 5 (Under construction)
The aims of the second hands on workshops in the second year are:
- introduce the resident to the clinical integration of IVC, lung and cardiac scanning
- introduce the resident to clinical problems for which a multi-scan approach should be pursued
- review the pitfalls of ultrasound findings and recognize circumstances in which the ultrasound findings should not be incorporated
III Senior resident teaching on CTU
Senior teaching will occur on a weekly basis when the resident is on resident is on a CTU rotation. When a PoCUS literate faculty member is available we will aim to provide one PoCUS session. The aims of the Senior teaching session will be to find a patient with pathology and demonstrate how PoCUS findings can be implemented clinically.
IV. Ultrasound and procedures rotation
This rotation is a standard 4 week block that runs at VGH and is open first to Senior residents. The rotation can accommodate up to 3 residents at a time. The rotation is meant to provide the resident with protected time to gain proficiency with PoCUS applications including ultrasound guided procedures. The residents on this rotation will receive weekly didactic and bedside instruction from one of the PoCUS faculty. They will have the opportunity to work on their bedside scanning on red patients that are admitted to the CTU at VGH. This provides a wealth of opportunity to scan normal anatomy, a variety of pathology and cutely unwell patients. The rotation activities and learning resources are also housed on the blackboard website.
The aims of the rotation are:
- consolidate ultrasound learning obtained during year 1
- provide multiple opportunities to become comfortable with bedside procedures
- help tach procedural skills to junior learners
- provide CTU teams with additional clinical information to assist with the diagnosis and management of difficult cases
Ultrasound and training resources
Residents in the UBC internal medicine residency program have easy access to ultrasound machines that are available for use on clinical rotations. Dedicated internal medicine point of care devices are kept on the internal medicine wards at all three major teaching hospitals. In addition, the program has ultrasound phantoms available for sim based procedure training. We also incorporate the Sonosim ultrasound simulator into the training program.

GE V-scan
I. Ultrasound machines
Vancouver General Hospital
- Cart based machines
- 2 X GE Venue 50 machines with 3 standard transducers
- Handheld machines
- 5 X GE V-scan with dual head transducer (1 machine for each CTU team)

GE Venue 50
Saint Paul’s Hospital
- Cart based machines
- 2 X GE Venue 50 machines with 3 standard transducers
Royal Columbian Hospital
- Cart based machines
- 1 Ultrasonix Touch with 3 standard transducers

Ultrasonix Touch
II. Ultrasound Training Resources
SonoSim computer based ultrasound simulator

Blue Phantom thoracentesis and CAE paracentesis task trainer


Online learning modules

Coming Soon: Telexy Q-Path archiving and QA platform

Textbooks
- Point of Care Ultrasound by Nilam J Soni, Robert Arntfield and Pierre Kory
- Introduction to Bedside Ultrasound Vol. 1 and 2 by Matthew Dawson and Mike Mallin
Podcasts and websites
- http://www.ultrasoundpodcast.com Matthew Dawson and Mike Mallin
- http://5minsono.com Jacob Avila
- https://westernsono.ca Robert Arntfield
- http://pie.med.utoronto.ca/POCUS/index.htm Toronto General Hospital Department of anesthesia
- http://www.thepocusatlas.com collaborative project to produce an image bank
- http://sonointernist.com Michael Wagner
Social Media
- @shanearish Shane Arishenkoff Internal Medicine UBC
- @irenema Irene Ma Internal Medicine U of C
- @ultrasoundpod Matt Dawson and Mike Mallin creators of ultrasoundpodcast.com
- @jminardi21 Joseph Minardi West Virginia University
- @thepocusatlas collaborative project to produce an image bank
- @jchristianfox Chris Fox University of California Irvine
- @5MinSono Jacob Avila creator of 5 minute sono
- @nobleultrasound Vicki Noble Emergency Medicine Case Western Reserve School of Medicine
- @BrisbaneLungUltrasound BLUE Team Brisbane Emergency Medicine Group
Examples of images from UBC Internal Medicine - click image or title for video
 |
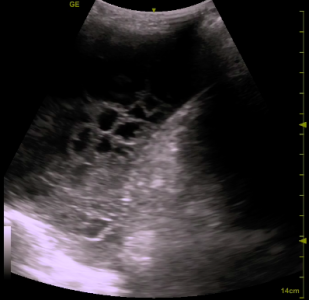
Complex pleural effusionThis is a coronal view of the posterior and inferior left hemithorax with the patient in the semirecumbent position. The anechoic space is pleural fluid. It is bordered by the diaphragm on the right and the lung intermittently on the left. The wavy, lattice-like hyper echoic strands are fibrin septations. Ultrasound is better than even a CT scan for characterizing these complex effusions. |
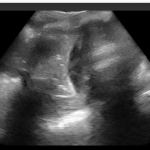 |
ConsolidationThis is a coronal view of the posterior and inferior left hemithorax with the patient in the semirecumbent position. The spleen and kidney can be seen to the right of the screen with the diaphragm coming in and out of view from behind a rib shadow in the middle of the image. The lung that is seen occupying the left aspect of the image has a soft tissue or hepatized appearance indicating that the airspaces have been replaced by fluid and exudate. Ultrasound is far superior than the chest x-ray for finding pneumonias. |
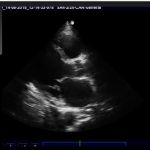 |
Severe LV systolic dysfunctionThis is a parasternal long axis of the heart with the LV lying to the left of the image. The LV is significant for the fact that there is almost know systolic myocardial thickening, very little change in the diameter of the chamber and the EPSS is approximately 2cm (visual estimation). The EF systolic function is severely impaired (<30%). Of note, one should never commit to an interpretation on a single view. The literature shows that internal medicine residents can quickly learn how to estimate ejection fraction with good accuracy. |
 |
Pericardial effusionThis is a parasternal long axis of the heart demonstrating a large (> 2cm in diastole) circumferential pericardial effusion. Note the concave appearance of the free wall of the RVOT throughout the cardiac cycle. This is evidence of RV collapse which suggests the possibility of tamponade. |
 |
Moderate hydronephrosisThis is a long axis view of the kidney demonstrating an anechoic space with 3 fingerlike projections that has replaced the normally hyper echoic renal pelvis. The dilatation of the major calyces is consistent with moderate hydronephrosis. Identifying this early on led to expedited management. |
POCUS Website
Check out the UBCIMPOCUS website, dedicated to promoting all things Point-of-Care Ultrasound